The literature is replete with studies showing the inexorable and undeniable link between mental and physical health. For an excellent overview of the relationship between mind and body, read the Robert Wood Johnson’s “Mental Disorders and Medical Co-Morbidity” written by Benjamin Druss and Elizabeth Walker, 2011. The paper cites data indicating that 25% of the adult population have a mental disorder and 58% had physical conditions. Of those with a mental disorder, 68% had co-occurring medical conditions.
In April, 2012, the National Survey on Drug Use and Health published data demonstrating the strong relationship between physical and mental health. Data showed that adults with mental illness were significantly more likely to have high blood pressure, asthma and stroke and more apt to utilize ER’s and hospitals than others. The Center for Integrated Health Solutions prepared a chart illustrating the strong link between physical and mental disorders. The National Association of Mental Health Program Directors recently published another excellent resource, “Morbidity and Mortality in People with Serious Mental Illness”.
Another overview exploring the relationship of psychiatric and physical disorders is “The Vital Link between Chronic Disease and Depressive Disorders”, by Daniel Chapman et al., 2005. Among other informative sources is the journal article “Depression and co-morbid medical illness: therapeutic and diagnostic challenges” by F. George Leon et al, Journal of Family Practice, Dec. 2003.
As part of California’s CalMEND program, Dr. Cheryl Cashin examined nonpsychiatric hospitalization rates among MediCal beneficiaries with serious mental disorders and found they had a significantly higher frequency, even relative to other high need populations. For a Powerpoint of her findings and data, go to “Excess Nonpsychiatric Hospitalization and Emergency Department Use among MediCal Beneficiaries“.

Taken from the World Health Organization, 2001, as presented by David Shern, 2008.
Here’s some of what the research in this area has shown:
- “People with serious mental illness treated by the public mental health system die on the average 25 years earlier than the general population; They live to 51, on average, compared with 76 for Americans overall. According to the data, they are 3.4 times more likely to die of heart disease; 6.6 times more likely to die of pneumonia and influenza, and 5 times more likely to die of other respiratory ailments.”
- C. Colton “Mortality: Health Status of the Served Population, Sixteen State Pilot Study on Mental Health Performance Measures”, based on 1997-2000 data.
- The 2001-03 Co-morbidity Survey Replication found that more than 68% of adults with mental disorders reported having at least one medical disorder and 29% of those with a medical disorder had a co-morbid medical condition.
- Alegria M, Jackson et al., National Co-morbidity Survey Replication (NCS- R), 2001-2003. Ann Arbor: Inter-university Consortium for Political and Social Research, 2003 as reported in “Mental Disorders and Medical Co-morbidity”, Robert Woods Johnson Foundation, 2011
- Among primary care clients with major depression, disabling chronic pain was present in 41% of those with major depression versus 10% of those without it.
- Bruce Arnow, “Comorbid Depression, Chronic Pain, and Disability in Primary Care”,Psychosomatic Medicine, 2006, 68.
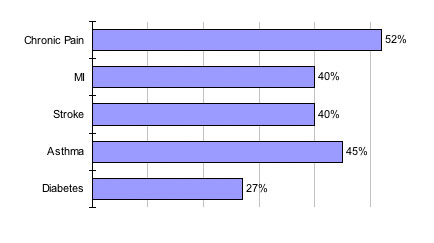
Prevalence of Depression with Other Chronic Diseases Percent with Depression (Pincus HA. J Clin Psychiatry. 2001;62 Suppl 6:5-9; Schatzberg AF. J Clin Psychiatry. 2004;65 Suppl 12;3-4.)
- Respondents reporting arthritis or rheumatism in a large-scale national survey also had an elevated prevalence of mood, anxiety and substance use disorders.
- Scott Patten et al., “Mental disorders in a population sample with musculoskeletal disorders”, BMC Musculoskeletal Disorders 2006, 7:37.
- “Primary care visits for patients with serious mental illness were more likely to be return visits, were longer, and were more likely to have scheduled follow-up than for clients without serious mental illness. Obesity, diabetes, and smoking were reported approximately twice as frequently in visits for patients with serious mental illness compared to patients without.
- Gail L. Daumit, “Characteristics of primary care visits for individuals with severe mental illness in a national sample”, General Hospital Psychiatry, 2002, Vol. 24, No. 6.
- “Based on analyzed insurance claims over a six year period, “persons with bipolar disorder were young (mean age, 38.8 years) and significantly more likely to have medical co-morbidity, including three or more chronic conditions (41% versus 12%, p < .001) compared with controls.”
- CP Carney, “Medical co-morbidity in women and men with bipolar disorders: a population-based controlled study”, Psychosomatic Medicine, 2006, 68 (5).
- Clients receiving previously unavailable mental health counseling lessened their use of nonpsychiatric, medical services by 39.7% and x-ray and lab services by 29.5%.
- [no author named], Kansas City Health Consumer, Feb. 1993.
- The addition of psychological interventions for Kaiser clients with serious medical disorders resulted in a 77.9% reduction in their average length of hospitalization; a 66.7% reduction in hospitalization frequency; a 48.6% decrease in number of prescriptions written; a 48.6% decrease in physician office visits, a 45.3% decrease in emergency room visits and 31.2% decrease in telephone contacts.
- R. Lechnyr, EAP (Employee Assistance Program) Digest), 1999 Nov/Dec.
- As compared with controls, patients with depression and co-occurring heart disease or diabetes who received collaborative care management had greater overall 12 month improvement in their level of hemoglobin, LDL cholesterol, systolic blood pressure and depression.
- Katon, W. et al., “Collaborative Care for Patients with Depression and Chronic Illness”, New Eng. Journal of Medicine, 363:27, 2010
- Seven of the ten leading causes of death (heart disease, cancer, stroke, chronic lower respiratory disease, accidents, diabetes and suicide) have a psychological and/or behavioral component.
- Centers for Disease Control and Prevention, 2005.
- Of the ten leading worldwide causes of disability, based on years lived with the disability, five are psychiatric or addictive conditions: major depression, schizophrenia, bipolar disorder, alcohol abuse, and obsessive compulsive disorder.
- Mental Health Report of the Surgeon General, 1999.
- An adverse physical health event substantially increases – by three times – the utilization of mental health care. Mental health service use increases with the severity of a physical health condition.
- Jangho Yoon et al., “The Role of Adverse Physical Health Events on the Utilization of Mental Health Services” Health Services Research, 2012
- Malignant melanoma patients who participated in group psychotherapy shortly after their diagnosis showed more enhanced immunological functioning after six months than did a similar group of melanoma patients who did not engage in group psychotherapy.
- F. Fawzy “Malignant melanoma: Effects of an early structured psychiatric intervention, coping, and affective state on recurrence and survival 6 years later.” Archives of General Psychiatry 1993, 50.
- In a study of emergency room patients with chest pain, nearly 41% met criteria for either an anxiety or depressive disorder as a primary medical diagnosis.
- K. Yingling, Gen. Internal Med. 1993, 8.
- Primary clients experiencing physical symptoms with a possible psychosocial component (e.g., palpitations, gastrointestinal disturbances, headaches, malaise, and sleep disorders) were randomly assigned to either behavioral interventions using didactic material, relaxation-response training, awareness training, and cognitive restructuring or to treatment focusing on information about stress management and its relation to illness. At six months, clients in the behavioral groups showed significantly greater reductions in medical visits and in discomfort from physical and psychological symptoms than did the clients in the information group.
- CJ Hellman, “A study of the effectiveness of two group behavioral medicine interventions for patients with psychosomatic complaints”, Behav Med. 1990, 16(4).
- Based on interviews and standardized tests, 44% of newly admitted cancer patients were given a psychiatric diagnosis and 3% had personality disorders. Approximately 68% of the psychiatric diagnoses consisted of adjustment disorders, with 13% representing major affective disorders (depression). Approximately 85% of those with a positive psychiatric condition were experiencing a disorder with depression or anxiety as the central symptom.
- L. R. Derogatis, “The prevalence of psychiatric disorders among cancer patients”, JAMA, 1983, Vol. 249, No. 6.
- Primary care clients with minor depression who were randomly assigned to an eight-week cognitive behavioral intervention experienced less somatic symptomatology associated with minor depression.
- J Miranda et al., “Intervention for minor depression in primary care patients”, Psychosomatic Medicine, 1994, Vol 56, Issue 2.
- A meta-analysis of ten studies involving 68,222 adults in England found that psychological distress is associated with an increased risk of mortality even at lower stress levels.
- Tom Russ et al., “Association Between Psychological Distress and Mortality: Individual Participant Polled Analysis of Ten Prospective Cohort Studies, BMJ, 2012
- Sixty percent of primary care clients with medically unexplained physical symptoms who were randomly assigned to a course of cognitive behavior therapy had physical symptoms rated as “very much” or “much improved” compared with only 25.8% of the usual care group. The intervention’s effect on these symptoms was greatest at treatment completion and persisted months after the intervention, although its effectiveness gradually diminished.
- Javier I. Escobar et al., “Effectiveness of a Time-Limited Cognitive Behavior Therapy-Type Intervention Among Primary Care Patients With Medically Unexplained Symptoms” Annals of Family Medicine 2007 (5).
- Based on primary care clients’ responses to select questionnaires, there was a strong association between somatic symptoms, whether medically explained or not, and “current psychological distress.”
- G. Simon, “Somatic symptoms of distress: an international primary care study”, Psychosomatic Medicine, 1996, Vol 58, Issue 5.
- Children who had 1-6 visits to a primary care-based psychological consultation service used medical services, especially acute primary care visits, less during the year after treatment, while a matched comparison group’s use was unchanged.
- Jack W. Finney, “Psychology in Primary Health Care: Effects of Brief Targeted Therapy on Children’s Medical Care Utilization” 1991, Journal of Pediatric Psychology 16(4).
- Older adults receiving enhanced care for depression experienced less pain due to arthritis and less interference with daily activities due to arthritis relative to a control group. Overall health and quality of life were also enhanced among intervention clients.
- Elizabeth Lin, “Effect of Improving Depression Care on Pain and Functional Outcomes among Older Adults With Arthritis” JAMA, 2003, Vol. 290, No. 18.
- The odds of depression in a diabetic group were twice that of the nondiabetic comparison group and did not differ by sex, type of diabetes, subject source, or assessment method.
- Ryan J. Anderson, “The Prevalence of Comorbid Depression in Adults with Diabetes” Diabetes Care, 2001, 24.
- “Depression is present in 1 of 5 outpatients with coronary heart disease and in 1 of 3 outpatients with congestive heart failure, yet the majority of cases are not recognized or appropriately treated.”
- Mary A. Whooley, “Depression and Cardiovascular Disease” JAMA, 2006;295.
- Major depressive disorder was found to be a risk factor for failure to achieve remission patients with active Crohn’s disease.
- P. Persoons et al., “The impact of major depressive disorder on the short- and long-term outcome of Crohn’s disease treatment with infliximab” Alimentary Pharmacology & Therapeutics, July 2005, Volume 22 Issue 2.
- Of 215 primary care clients who scored high on a depression scale, 80% made “somatic presentations”.
- L.J. Kirmayer et al., “Somatization and the recognition of depression and anxiety in primary care”,Am J Psychiatry 1993; 150.
- Clients aged 60 and older with major depressive disorder who were randomly assigned to an intervention designed to improve mood experienced significantly better physical functioning at one year compared with usual-care clients and were less likely to rate their health as fair or poor (37.3% vs 52.4%, P <. 001).
- Christopher M. Callahan et al., “Treatment of Depression Improves Physical Functioning in Older Adults”, J Am Geriatr Soc. 2005, 53(3).
- A study involving 6,865 persons found that patients with mental illness had an average of 5.2 ER visits compared to 2.5 visits for those without mental illness” and that cocaine users with mental illness were 3.5-times more likely to visit the ER four or more time compared with users without mental illness.
- Geoffrey Curran et al., “Mentally ill drug abusers Have More ER Visits”, BMC Emergency Medicine, 2008
- About 88% of persons with schizophrenia smoke, three times the rate of the general population.
- J. Hughes, Prevalence of Smoking Among Psychiatric Outpatients:, Amer Journal of Psychiatry, 1986, 143.
- A study involving 6,865 persons found that patients with mental illness had an average of 5.2 ER visits compared to 2.5 visits for those without mental illness” and that cocaine users with mental illness were 3.5-times more likely to visit the ER four or more time compared with users without mental illness.
- Geoffrey Curran et al., “The Association of Psychiatric Co-morbidity and Use of the Emergency Department among Persons with Substance Abuse Disorders: An Observational Cohort Study”, BMC Emergency Medicine, 2008 (1) 17.
- Pain was present in 2/3’s of 573 clinically depressed primary care patients and its severity was a strong predictor of poor depression and health-related quality of life outcomes at three months, despite anti-depression therapy.
- M. Bair et al., “Impact of Pain on Depression Treatment Response”, Psychosomatic Medicine66.77, 2004
- A meta-analysis of published research on the disease risk in people with severe mental illness concluded that there was a significant higher incidence of diabetes in this population.
- D. Osborn et al., Relative risk of diabetes, dylpidaemia, hypertension and the metabolic syndrome in people with severe mental illness: systematic review and metaanalysis”, BMC Psychiatry 8:84, 2008
- Sixty percent of premature deaths in persons with schizophrenia were due to medical conditions such as pulmonary, infectious and cardiovascular diseases.
- J Parks et al., “Morbidity and Mortality in People with Serious Mental Illness”, written for the National Association of State Mental Health Directors, 2006.
- Total cancer incidence for adults with schizophrenia or bipolar disorder was 2.6 times higher than found in other Medicaid adult beneficiaries.
- Emma McGinty et al., “Cancer Incidence in a Sample of Maryland Residents with Serious Mental Illness”, Psychiatric Services, 2012, Vol. 63, No. 7.
- People with serious mental illness treated by the public mental health system die on the average 25 years earlier than the general population; They live to 51, on average, compared with 76 for Americans overall. According to the data, they are 3.4 times more likely to die of heart disease; 6.6 times more likely to die of pneumonia and influenza, and 5 times more likely to die of other respiratory ailments.
- C. Colton “Mortality: Health Status of the Served Population, Sixteen State Pilot Study on Mental Health Performance Measures”, based on 1997-2000 data.
- Persons with schizophrenia have an increased chance of having diabetes and diabetic complications.
- C. Carney et al., “Medical Co-Morbidity in Women and Men with Schizophrenia” J of General Internal Med 2006, 21.
- “Fifty percent of all care for primary care patients with mental disorders is delivered solely by general medical practitioners” (based on other cited epidemiological studies).
- K. Strosahl, “Building Primary Care Health Delivery Systems that Work: A Compass and a Horizon”, in Behavioral Health in Primary Care: A Guide for Clinical Integration, pgs 37-58, 1997.
- Anxiety and depression are common in patients hospitalized for coronary angiography and “each was independently associated with an approximate 2-fold increased risk of all-cause mortality. The association of these factors was additive with a 3-fold increased risk in anxious patients with co-morbid depression.”
- Watkins, L. et al., . “Association of Anxiety and Depression with All-Cause Mortality in Individuals with Coronary Heart Disease:, J. Am. Heart Association, 2013, 2
